CORNEA
Cornea is transparent outlayer of the eye, in front of iris and pupil which covers the eye. It is extremely sensitive to even minimal damages, because of very rich innervation.
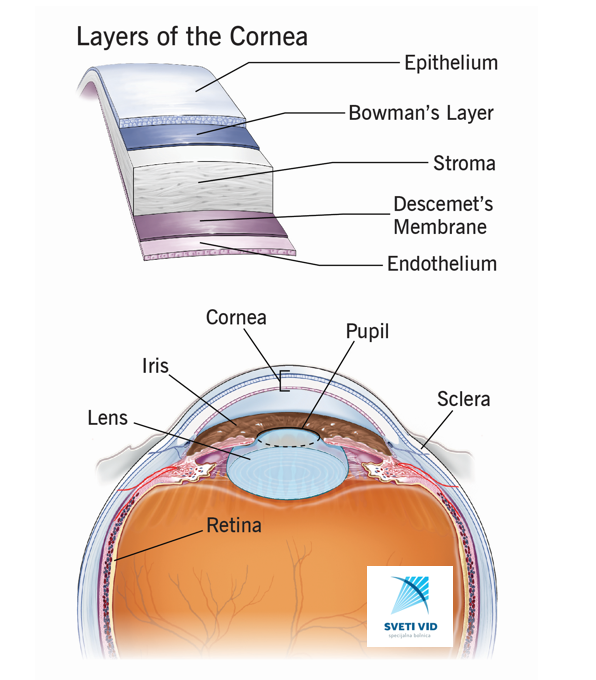
There are no blood vessels in cornea and that is why cornea is transparent. The nutrients supply comes from humour aqueous. There are 6 layers of cornea(the 6th layer was recently discovered and named Dua layer according to the author and it is situated between descent membrane and stroma).
Moisturising of cornea is very important for keeping cornea in good condition and that is why tear film has essential role in that process.
This anterior part of cornea is mechanical protection of the eye from environmental influence with keeping architecture of cornea in good condition.
The optical characteristics of cornea are focusing and refracting of the light rays. Dioptric power of cornea is 2/3 of total dioptric power of the eye.
Healthy and transparent cornea as well as healthy tear film are conditions for a good sight.
Corneal damages can present in the following features:
-corneal shape and curvature changes
-losing of transparency
-swelling
-scars
-opacities
-erosions
-thinning
-ulceration
-threatening corneal rupture
CONDITION THAT CAN LEAD TO CORNEAL DAMAGE
-inherited corneal dystrophies
-infections
-trauma
-earlier surgeries
-neurologic disease
-keratitis
-systemic diseases
-glaucoma
-long usage of some eyedrops containing benzalkonium chloride
-tear film damage, Meibomian glandes disease(MGD)
-dry eye (keratitis sicca)
In highly damaged cornea with visual loss, corneal transplantation must be done.
CORNEAL TRANSPLANTATION
Corneal transplantation/keratoplasty/ is a surgical procedure by which the damaged cornea is replaced with healthy donor cornea.
In recent 10 years this surgical procedure has been developed. The advantages in these new surgical procedure are in possibilities to change the whole cornea (PK) or partially, only the damaged layer depending on the type and grade of lamellar damages. PKP (perforative keratoplasty) means the exchange of the full-thickness cornea, in cases when the cornea is highly damaged, with deep and large scars, central leucoma, very thin cornea and threatening corneal ruptures. The recovery is long, high postoperative astigmatism due to the whole circumference cut and sutures, high risk of graft rejection.
The partial keratoplasty (lamellar), as less invasive, has advantages in faster recovery and lower risk of graft rejection. These are endothelial and deep anterior lamellar keratoplasty.
A) Endothelial keratoplasty means exchange of deeper inner layer of cornea with a healthy disc tissue of donor. Anterior stroma stays. Indications are endothelium damages, dystrophies(most often Fuch`s).
-DSEK (includes the thin inner layer of stroma with descement and endothelium)
-DMEK (slightly thinner than DSEK-includes descement and endothelium only).
B) Deep anterior lamellar keratoplasty (DALK)
DALK means exchange of outer anterior layer of central cornea with a healthy graft tissue. Endothelium and descement stay.
THE RISKS OF CORNEAL TRANSPLANTATION
-bleeding
-lamella/graft dislocation or detachment
-inflammation
-refractive error (astigmatism)
-higher intraocular pressure because of postoperative therapy (secondary glaucoma)
-anterior and deep ocular infection (ulcus hypopion endophthalmitis)
-rejection of the graft
The immune system recognizes the donor tissue as foreign and creates immune response to reject the new cornea. That risk stays forever.
There are many factors that influence the rejection:
-age
-outlined disease
-the previous diseases (operations, trauma etc.)
-medications
The causes of corneal impairments:
-herpes
-vascularised leucoma (trauma)
The studies have shown that the rejection mostly comes from the patient himself because of not obeying the strict therapeutic regimen and follow-ups, as well as not announcing early symptoms of rejection, that they have been informed about before. The graft rejection is mostly reversible but with prompt beginning of therapy.
WARNINGS
If in postoperative period you notice any change in visual acuity, pain, irritation, redness, blurred vision, enhanced light sensitivity IMMEDIATELY CONTACT THE HOSPITAL NO MATTER WHEN THE TERM OF YOUR PLANNED CONTROL IS.
The symptoms that you feel may be the sign of rejection beginning and only with the prompt intervention that could be stopped. Please check if you had missed some drops maybe. The rejection of corneal transplant most often happens when the patient does not use the prescribed therapy regularly. Phone the hospital and maybe you would be suggested to use the therapy on stronger regimen or to add some other drops.
THERAPY
Immediately after the operation, you would be prescribed antibiotics and corticosteroids against infection, pain and swelling.
Controls are the day after the operation, then in first week more often, and then monthly on 3 months.
In postoperative follow-ups, the therapy could be changed according to the findings. In some cases it is possible to include some stronger drugs (cyclosporin, MTX etc.)
This therapy is used for a longer period of time and that is why it is necessary to control laboratory findings during this period.
WHAT IS EXPECTED AFTER CORNEAL TRANSPLANTATION?
Mostly it is an outpatient surgery, but sometimes the doctor can ask for staying in hospital during the night. You will have protective eye shield over the operated eye, only as a mechanical protection. Anesthesia could be local or general, determined by the surgeon. The vision would be blurred for a while. It is expected increased feeling of light sensibility and some kind of discomfort. It could be painful the day after the surgery, especially in perforative keratoplasty(PK) because of the large corneal cut and suturing.
In lamellar keratoplasty is mandatory to stay laying on the back (back sleepers) immediately after the surgery and to proceed with that for a while, depending on the surgeon`s suggestion, with very few short breaks during the day.
In lamellar keratoplasty the air bubble is applied in anterior chamber to keep the lamella on place, because of sutureless surgery.
So the outcome of the surgery highly depends on how the patient follows these rules.
Use your therapy as suggested regularly, take care about hygiene and be responsible to yourself.
It is forbidden to rub and to make a pressure on the eye.
Even non-contact IOP measuring is forbidden for several months.
Very demanding and complicated surgery has just been done and it is important to take care about this postoperative period very cautiously, so that the complications would be avoided:
-from now on, you should accept the new way of living with transplanted cornea, and avoid in the future any situations with possible risk of injuries (group sports-basketball, football, jumping in the water, tennis,…).
-in the first 3-4 months avoid gym and heavy physical jobs
-you should be back to office work after couple of weeks (after partial keratoplasty) and a couple of months (after total keratoplasty (PK))
-avoid places of possible air-contamination and infections
-do not drive by yourself for a few weeks after the surgery (unless the doctor says differently)
-after the operation the vision would be blurred and after the therapy by time it would clear up
-you would feel sometimes fluctuations in visual acuity until the situation stabilizes.
-for a complete recovery, you will need a few months (for lamellar keratoplasty) and even a year or maybe more (for total keratoplasty)
-the sutures in total keratoplasty would be removed after approximately a year after the operation
-postoperative astigmatism is expected to change after the suture removing
ARTIFICIAL CORNEA – WHEN CORNEAL TRANSPLANTATION IS NECESSARY BUT NOT POSSIBLE?
Artificial cornea is used in cases of large scars and complete corneal damage with vascularisation, mostly after trauma when with corneal transplant bad outcome and rejection of the graft would be expected.
WHEN COULD CORNEAL TRANSPLANTATION BE AVOIDED?
1.CXL – corneal cross linking
Inherited corneal dystrophies often have late manifestations after 20`s. They start with irregularities in corneal curvature – astigmatism and thickness of cornea.
Some of these cases (keratoconus) with corneal cross linking procedure could be successfully treated before advanced clinical manifestations.
The earlier procedure done (with first symptoms), the better the outcome would be and cornea and sight would be preserved and transplantation avoided.
That is why, owing to CXL, nowadays corneal transplantation in keratoconic corneas is rarely used.
However, corneal transplantation must be done in advanced keratoconic corneas when it is too late and cornea is too thin for CXL.
The crucial thing is early detection of first, even preclinical changes in cornea, and doctor has responsibility to recognise keratoconus on time and suggest the procedure. Fortunately, with contemporary imaging diagnostics, it is impossible to overmiss the diagnosis.
2.EXCIMER LASER – PTK (photo therapeutic keratectomy)
PTK is used in removing of small and superficial corneal opacities or scaring, as well as fast and regular corneal healing in the cases of recidivant corneal erosions.
Corneal erosions are very painful and PTK leads to faster healing and symptomatic relieves.